19 Key Differences between Passive Immunity and Active Immunity
Immunity is the capacity of a multicellular organism's body to defend itself against foreign substances and infectious agents by having the capacity to obliterate them in order to avoid contracting new diseases.
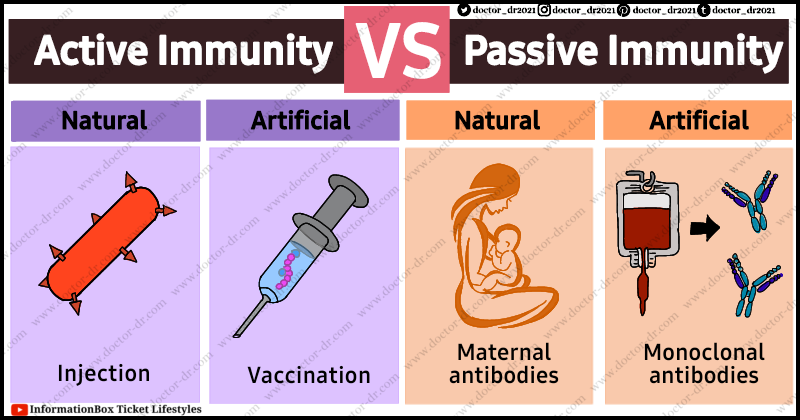
Either active or passive vaccination can provide protection against contagious bacteria. Immunity can be developed in each case either naturally (often by transmission from mother to foetus or through earlier infection by the organism) or artificially, such as through the injection of antibodies or vaccinations.
An immune system enables the body to resist infections. Innate immunity and adaptive immunity are the two main types of protection that make up immunity.
The human body's initial line of protection is called innate immunity. It is an innate (present at birth) or inherited immune protection system. Internal or external defence are both possible forms of innate immunity. The body's external defence, which includes the skin, tears, and stomach acid, strives to prevent exposure to infections. Internal defence, sometimes referred to as the second line of defence, consists of fever, inflammation, and phagocyte defensive systems.
The third layer of defence, which is triggered by innate immunity, is adaptive immunity, also referred to as acquired immunity. The immune response is triggered by the host's reaction to a foreign antigen (pathogen), or by the transfer of antibodies or lymphocytes that are particular to the pathogen. This form of immunity and the immunological responses generated are acquired only through experience. It involves the immune system's protection as well as that of other activated substances like cytokines. The body is guarded by this form of protection against certain viruses.
Active immunity and passive immunity are two categories for adaptive immunity.
Table of Contents
- Active Immunity vs Passive Immunity Table Form
- Combined Active and Passive Immunity
- Other forms of Immunity
- Local Immunity
- Herd Immunity
Active Immunity vs Passive Immunity Table Form
|
S.N. |
Characteristics |
Active Immunity |
Passive Immunity |
|
1. |
Definition |
The form of immunity that
serves as protection and involves activating a person's own immune system to
manufacture antibodies and lymphocytes. |
immunity in which a person
obtains antibodies or lymphocytes produced by the immune system of another
person. |
|
2. |
Exposure to Antigen |
Requires being exposed to a pathogen or its antigen. |
Does not require exposure to an infectious agent or its antigen. |
|
3. |
Immune system involvement |
The person's immune system is
actively involved in the process. |
The person's immune system is
not participating actively, but rather passively. |
|
4. |
Natural acquirement |
Arise naturally when an individual is exposed to an antigen or
pathogen (clinical infection). |
arise spontaneously when a nursing newborn consumes antibodies
from the mother's milk or when a foetus absorbs antibodies from the mother
through the placenta. |
|
5. |
Artificial acquirement |
Conferred artificially by
means of vaccines. |
Conferred artificially by
administration of preformed antibodies. |
|
6. |
Immunity type |
Involves both humoral and cell-mediated immunity. |
The immunity is conferred only by readymade antibodies. |
|
7. |
Components |
T cells (cytotoxic T cells),
B cells (memory B cells and plasma cells), and antigen-presenting cells
(helper T cells, memory T cells, and suppressor T cells) (B cells, dendritic
cells, and macrophages). |
No immune cells are involved
as the antibody is preformed. |
|
8. |
Antibody production |
Involves antibody production which is induced by infection or
immunogen. |
No antibody is produced but directly transferred. |
|
9. |
Memory cell formation |
Active immunity induces the
development of durable memory cells.. |
Memory immune cells are not
formed. |
|
10. |
Secondary response |
If a person is exposed to the same pathogen again later, a
significantly quicker and stronger secondary response is generated after the
initial exposure. |
Absence of a secondary response. |
|
11. |
Durability |
The protection offered is
long-lived. |
The protection is only
transient. |
|
12. |
Response time |
Due to the lag period, the protective reaction takes some time
to become established. |
No lag period hence the protection is instant. |
|
13. |
Reactivation |
Reactivated by the recurrence
of infection or by revaccination. |
Frequent re-administration is
needed for renewed protection. |
|
14. |
Booster effect |
Subsequent doses with antigens cause booster effects. |
Subsequent doses are less effective due to immune elimination. |
|
15. |
Suitability |
Immuno-deficient or immuno-compromised
people cannot be protected by active immunity. |
In conditions of
immunosuppression, immunodeficiency, or severe combined immunodeficiency,
passive immunity is helpful. |
|
16. |
Use |
Very effective for prophylaxis of diseases. |
Artificial passive immunity is effective as a post-exposure
remedy. |
|
17. |
Effectiveness of Protection |
Provides effective
protection. |
Protection rendered is less
effective and may not be complete. |
|
18. |
Adverse effect |
It can be implicated in autoimmune diseases and allergies, but
generally does not have side effects. |
A condition called serum sickness can result from exposure to
antisera. |
|
19. |
Examples |
Natural – Producing antibodies in response to exposure to a pathogenic
infection such as measles or cold. Artificial – Producing antibodies in response to the controlled exposure to
an attenuated pathogen (i.e. vaccination). |
Natural – Receiving antibodies from another organism (e.g. to the
fetus via the colostrum or a newborn via breast milk). Artificial – Receiving manufactured antibodies via external delivery (e.g
blood transfusions of monoclonal antibodies). |
Combined Active and Passive Immunity
Giving both preformed antibodies (antiserum) and a vaccination to give short-term and long-term protection, respectively, against a disease is known as combined passive-active immunity. This strategy is used to prevent the spread of tetanus, rabies, and hepatitis B, among other infectious diseases.
Another possibility is that a person who has been bitten by a rabid animal could get a rabies vaccination and rabies antibodies (passive immunisation to produce an instant reaction) (active immunity to elicit a long-lasting response to this slowly reproducing virus).
Other forms of Immunity
Local Immunity
- Local immunity refers to the defences in place at a specific location, typically where a pathogen invades and multiplies.
- Secretory IgA antibodies in different bodily secretions provide local immunity.
- Local plasma cells found on mucosal surfaces or in secretory glands generate these antibodies.
- Local immunity is induced in the gut mucosa and nasal mucosa, respectively, by naturally occurring infection or attenuated live virus vaccines administered orally or intranasally.
Herd Immunity
- When enough people in a community have been exposed to a disease, there is a general degree of protection known as herd immunity, which prevents the infection from spreading quickly.
- With herd immunity, the disease will have a smaller pool of people to infect and cause fewer outbreaks within the population as more people grow immune.
- Sometimes the ability of the population as a whole to establish strong herd immunity to the pathogen is necessary for the eradication of an infectious illness. When herd immunity is very low, which indicates that there are more vulnerable individuals in the population, an epidemic of a disease is more likely to develop.
- However, not all infections spread as quickly, and different levels of community immunity are required to take advantage of herd immunity.
- For instance, a community needs practically everyone to be immune to limit the spread of measles because it is one of the most infectious viruses known. However, compared to most other infectious diseases, it is far more challenging for an individual to gain from herd immunity to the measles. As a result, vaccinations have made it simpler for society to benefit from this kind of protection.
- Researchers have argued over herd immunity and COVID-19, arguing that it may be attained by natural infection but would have negative effects and is, thus, not a solution to immunity to COVID-19.