- A strain of E. coli is considered to be enterotoxigenic if it produces at least one enterotoxin from either the heat-stable toxin (ST) or the heat-liable toxin (LT) groups.
- Thus, the term "Enterotoxigenic Escherichia coli," or "ETEC," refers to a particular kind of E. coli that generates unique toxins that stimulate the lining of the intestines and cause it to discharge an excessive amount of fluid, which results in diarrhoea.
- ETEC strains are still known to infect newborn animals with a deadly form of diarrheal illness, which was initially identified as being caused by piglets.
- Serotypes 06, 08, 0 15, 025, 0 27, 0 153, 0 159, and others are frequently linked.
Disease Caused
- One of the most frequent causes of bacterial diarrheal disease in developing nations is enterotoxigenic E. coli (ETEC), which is also responsible for approximately 30% of diarrheal travellers to these nations.
- In developing nations, the illness is known as traveler's diarrhoea and weanling diarrhoea (infant diarrhea).
Mode of Transmission
Most commonly, the infections are contracted by consuming feces-contaminated food or water. There is no spread from person to person.
Toxins and Pathogenesis
- Heat-stable (ST) and heat-labile (LT) enterotoxins mediated by plasmids that promote fluid and electrolyte hypersecretion
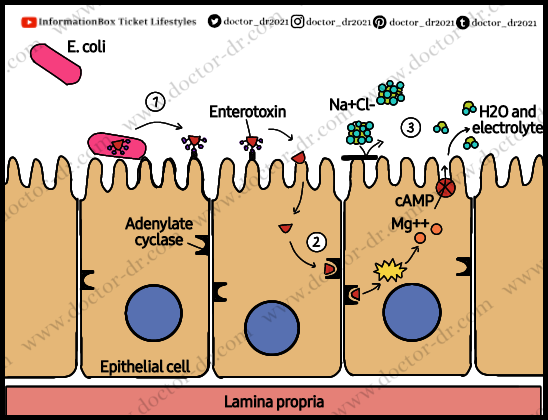
- The organisms develop their plasmid-encoded enterotoxins and colonise the small intestinal mucosa, resulting in a net secretory condition.
- Enterotoxins LT and ST work together in ETEC strains to produce diarrhoea. These strains may express LTs exclusively, STs exclusively, or both LT and STs.
- In order to cause disease, bacteria must adhere to the small intestinal epithelium via colonisation factors (CF) and produce heat-stable and heat-labile enterotoxins.
- On a transmissible plasmid are the genes for the enterotoxins and colonisation factors encoded.
- The most prevalent colonisation factors are CFA/I, CFA/II, and CFA/IV, which are further separated by their antigenic characteristics (coli surface antigens [CS]). More than 20 CS colonisation factors have been identified, and the affinity of these factors for host cell receptors determines their host specificity.
- Enterotoxins produced by ETEC fall into two categories: heat-stable (STa and STb) and heat-labile (LT-I, LT-II).
- Heat-resistant toxins Only connected with human sickness, present in 75% to 80% of ETEC either by itself or in combination with LT, STa is more frequently linked to severe illness than LT-only ETEC strains.
- A small monomeric peptide called STa binds to the intestinal epithelium's transmembrane guanylate cyclase C receptor. This causes a rise in cyclic guanosine monophosphate (cGMP), which triggers fluid hypersecretion and inhibits fluid absorption.
- Of the heat-labile toxins, LT-I is most frequently linked to illness in people. With 80% structural and functional similarities to cholera toxin, LT-I has one A subunit and five identical B subunits.
- The B subunits bind to the same receptor (GM1 gangliosides) as cholera toxin and other surface glycoproteins on small intestinal epithelial cells. The A component travels across the vacuolar membrane during endocytosis and interacts with the membrane protein Gs to control adenylate cyclase. The overall upshot of this interaction is a rise in cyclic adenosine monophosphate (cAMP) levels, which leads to increased chloride secretion and reduced salt and chloride absorption. Watery diarrhoea is one of these alterations.
- Prostaglandin secretion and the creation of inflammatory cytokines are also stimulated by toxin exposure, leading to further fluid loss.
Signs, Symptoms, and Complications
Within 1-3 days of exposure, illness sets in, with symptoms seldom lasting more than 3 weeks.
- The identifying signs include:
- Bloodless and watery diarrhoea
- stomach pains
- vomiting and nausea are less frequent
Although mortality is higher in those who are undernourished and those who have underlying conditions, especially children and the elderly, the symptoms are comparable to those of cholera but typically milder.
Diagnosis
For a long time, finding the enterotoxins LT and/or ST was the only reliable method of finding ETEC.
- There are commercial immunoassays that can identify ST in clinical samples and cultures.
- PCR tests performed on clinical samples.
Treatment
Typically, the sickness lasts 3 to 4 days. It could take a week or more for certain infections to go away. The majority of people heal on their own and don't need hospitalization or antibiotics.
Prevention
- Avoiding or properly cooking meals and drinks that can be contaminated with the germs, as well as routinely washing your hands with soap, might help prevent infection.
- For travelers in developing countries, ETEC infection can be prevented by avoiding foods and beverages that could be contaminated with bacteria.




.webp)