Table of Contents
4. Molecular Rigidity and Complexity
5. Antigenic Determinants and Cross-reactivity
1. Types of antigen-based on their origin
2. Types of antigens on the basis of immune response
1. Endogenous Pathway or Classical MHC class I Presentation
2. Exogenous Pathway/ Classical MHC class II Presentation
Antigen Definition
Antigens are molecules or molecular structures that the body does not recognise and which often cause the formation of antibodies as a result of an immunological response.- In simple words, antigens can be anything that doesn’t belong to the body and are foreign.
- Although the generation of an immune response is typically used to characterise antigens, this is not always the case. Immunogens are the antigens that cause a reaction.
- Antigenic determinants, or certain areas on antigens known to induce an immune response, are necessary for antigens to do so. To trigger a reaction, the determinants attach to receptor molecules on immune cells that have a complementary structure.
- The name "Ag" denotes antigens, which can exist as bacteria, viruses, chemicals, pollen, or other substances.
- The ability of our body to discriminate between internal parts of the body and external particles gave rise to the idea of an antigen.
- The body produces antibodies that work against these antigens in response to these antigens.
- Proteins, peptides, and polysaccharides make up the majority of human antigens; however, lipids and nucleic acids can also function as antigens when mixed with proteins or polysaccharides.
- In order to activate the body's adaptive immune system against the antigen, antigens may also be purposefully injected into the body in the form of vaccinations.
Properties of Antigens
Antigens have a variety of characteristics that affect their immunogenicity, making them crucial for comprehending the immune response to them. These qualities are regarded as necessary to create a good antigen since they determine immunogenicity. The following are a few characteristics of antigens:
1. Foreign Nature
- All antigens that cause the host to mount an immune response are external to the recipient's body.
- The antigen is recognised by the host body as being distinct from the regular bodily parts.
- With an increase in the level of foreignness, the antigen's immunogenicity rises. When it comes to biological antigens, the alienness grows as the evolutionary distance between the two species widens.
- There are certain exceptions, though, in that some proteins produced by the host may also trigger an immune response, as is the case with autoantigens.
- Similar to this, if proteins or other molecules from different species lack antigenic determinants or epitopes, they can similarly fail to elicit an immune response.
2. Chemical Nature
- Proteins and polysaccharides are the most powerful and often encountered antigens.
- Yet, when they combine with proteins and polysaccharides, other compounds including lipids and nucleic acids can also function as antigens.
- For proteins, the immunogenic portions of the antigen must have at least 30% of amino acids such as lysine, glutamine, arginine, glutamic acids, asparagine, and aspartic acid, as well as a significant amount of hydrophilic or charged groups.
- With the heterogenicity of the molecules, the amount of immunogenicity likewise rises. Generally speaking, homopolymers are less immunogenic than heteropolymers.
3. Molecular Size
- The immunogenicity of the molecules is also greatly influenced by the antigens' molecular sizes.
- Antigens must be at least 5000 Da in size in order to qualify as immunogenic, according to accepted standards.
- Yet, when combined with big transporters, compounds with low molecular weight might exhibit immunogenicity.
- Haptens, or compounds with low molecular weight and at least one antigenic determinant, are regarded as "partial antigens."
4. Molecular Rigidity and Complexity
- Molecules' stiffness and complexity are crucial aspects that affect their immunogenicity.
- In comparison to less rigid molecules, those that are stiff may produce antibodies to specific structures, making them ideal antigens in general.
- The complexity of the structure is also important since peptide antigens with repeating units of only one amino acid are less immunogenic than those with repeating units of two or more amino acids.
5. Antigenic Determinants and Cross-reactivity
- Antigenic determinants are parts of an antigen molecule that have a role in how antibodies respond with them.
- Antigens having two or more antigenic determinants typically can stimulate the formation of antibodies. Because a tiny molecule cannot have more than one antigenic determinant, a smaller antigen often does not cause the formation of antibodies.
- The ability of antibodies produced in response to one antigen to interact with another antigen is known as cross-reactivity of antigens.
Antigen Structure
- The capacity of an antigen to attach to the antigen-binding site of an antibody defines its molecular structure.
- Antibodies distinguish between various antigens based on the distinctive molecular structures that each antigen has on its surface.
- The majority of antigens are polysaccharides or proteins. They can be the caps, flagella, poisons, fimbriae, and coats of many bacteria, viruses, and microorganisms. Furthermore, secretions and other substances of a similar origin can function as antigens.
- These microbes' lipids and nucleic acids are only immunogenic when coupled with proteins or polysaccharides.
- Depending on the kind, size, and immunogenicity of the antigen, it may have a distinct shape.
- Every immunogenic antigen possesses an exclusive structural element known as an epitope or an antigenic determinant.
- The amount of epitopes varies between antigens and affects how many antibodies may bind to a particular antigen.
- Different structural elements of interaction in antigens dictate the kinds of antibodies that they bind to.
- A paratope is the area of an antibody that interacts with an antigen. It has been determined that because the structures of an epitope and a paratope are distinct and complement one another, they may both be described as locks and keys.
Types of Antigens
Depending on a variety of variables, antigens can be divided into many categories. Based on the antigen's immunogenicity and place of origin, certain categories are frequently used.
1. Types of antigen-based on their origin
Antigens can be classified into two groups on the basis of their origin;
a. Exogenous Antigens
- Exogenous antigens are those that come from outside the host's body and are thus unfamiliar to the host.
- These antigens may be ingested, injected, or inhaled into the body; they then travel throughout the body via bodily fluids.
- Antigen Processing Cells (APCs), such as macrophages and dendritic cells, play a major role in the phagocytosis that is the primary mechanism for the absorption of foreign antigens.
- Many antigens, including intracellular viruses, may start off as foreign antigens before evolving into endogenous antigens.
b. Endogenous Antigens
- Endogenous antigens are those that develop naturally in the host's body as a result of intracellular bacterial or viral infection or during metabolism.
- Endogenous antigens are typically found in the body's cells or in the fragments, substances, or metabolic byproducts that are antigenic.
- Normally, they are handled by macrophages before being found by cytotoxic T-cells in the immune system.
- Xenogenic or heterologous, autologous, and idiotype or allogenic antigens are examples of endogenous antigens.
- Due to the host immune system's recognition of its own cells and particles as immunogenic, endogenous antigens may cause autoimmune disorders.
Autoantigens
- Autoantigens are host proteins or protein complexes that the immune system of the host attacks, leading to autoimmune illness.
- While the immune system shouldn't attack the body's own cells, autoantigens might be fatal to the host.
- Genetic and environmental factors cause the loss of immune tolerance to such antigens.
Tumor Antigens (Neoantigens)
- Major Histocompatibility Complex (MHC) I and II present tumour antigens or neoantigens on the surface of tumour cells.
- The tumor-specific mutation that occurs during the malignant transformation of normal cells results in the production of the antigens.
- Due to the tumour cells' ability to escape antigen presentation and immune defence, these antigens often do not elicit an immunological response.
Native Antigens
- Native antigens are antigens that have not been altered by any antigen-presenting cells (APCs), making them inaccessible to immune cells like T-cells.
- Yet, even without any processing, such antigens can activate B-cells.
2. Types of antigens on the basis of immune response
Based on the immunological response, there are two main categories of antigens;
a. Complete antigens/ Immunogens
- Complete antigens, also known as immunogens, are antigens that cause a particular immune reaction.
- These antigens don't require any carrier particles to elicit an immune response.
- They are often high molecular weight proteins, peptides, or polysaccharides (greater than 10,000 Da).
b. Incomplete antigens/ Haptens
- Antigens that are incomplete, also known as haptens, are unable to elicit an immune response on their own.
- Typically, a carrier molecule is needed for these non-protein compounds to fully develop into an antigen.
- Few antigenic determinant sites and a low molecular weight (often less than 10,000 Da) characterise haptens.
- The carrier molecule, which is either a protein or a polysaccharide molecule, is attached to the hapten and is regarded as a non-antigenic component.
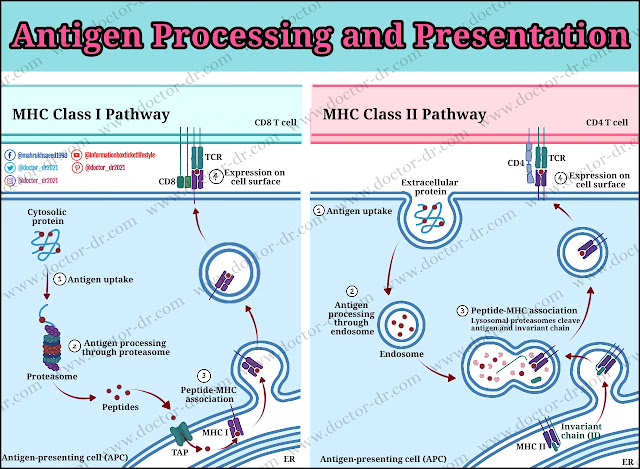
Antigen Processing and Presentation
Antigen-presenting cells (APCs) break down antigens into smaller peptide fragments, which are subsequently presented on the surface of the cells via antigen-presenting molecules like MHC class I and II to be recognised by lymphocytes.
Antigen processing and presentation can occur via three different pathways;
1. Endogenous Pathway or Classical MHC class I Presentation
- The endogenous pathway of antigen processing and presentation utilizes mechanisms similar to those involved in the normal turnover of intracellular proteins.
- The proteasome, a specialised cytosolic proteolytic mechanism, is used by the antigen-presenting cells to break down the protein antigen into short peptides.
- The immunoproteasome, which is involved in the immune system, contains components that are activated by exposure to interferon or TNF.
- The aminopeptidases in the ER lumen trim peptides as the next step in the proteolytic processes.
- The Transporter Associated with Antigen Processing carries the peptides produced by proteolysis to the ER lumen (TAP).
- The loading and trimming of peptides on MHC class I molecules is mediated by TAP, tapasin, and the calnexin-calreticulin system in addition to TAP.
- MHC class I molecules will either be delivered to the cell membrane or recycled by a process reliant on UDP-glucose glycoprotein transferase-1, depending on the affinity of the loaded peptides.
- In the case of high-affinity MHC class-1 complexes, the peptides are delivered to the cell membrane via the Golgi apparatus in order to stimulate CD8+ T cell responses that are specific for the antigen.
2. Exogenous Pathway/ Classical MHC class II Presentation
- In the exogenous route, the antigen is internalised by APCs by straightforward phagocytosis once the substance interacts to certain surface receptors.
- The endocytic processing pathway uses the compartments of the cell to break down proteins into peptides.
- The internalised antigen passes through several acidic compartments, where it comes into contact with hydrolytic enzymes and low pH.
- The MHC class II-containing compartment (MIIC), which is specific to the APCs, is where the ultimate protein breakdown and peptide loading occur.
- As APCs express both classes of MHC, a unique mechanism exists to stop antigenic peptides from interacting with class I molecules.
- The class II chains connect with a protein known as the invariant chain during the synthesis of class II MHC molecules. This protein blocks endogenously produced peptides from attaching to the class II molecule by interacting with the groove that binds class II peptides.
- The invariant chain deteriorates as it passes through several compartments, eventually forming a brief piece known as CLIP (class II-associated invariant chain peptide).
- Afterwards, an exchange of CLIP with an antigenic peptide is catalysed by a class II MHC protein.
- The class II MHC molecules' stability and structural integrity depend on the peptide binding.
- The class II MHC -peptide complex is transported to the plasma membrane once the peptide has been bound, where the neutral pH induces the complex to form a compact, stable form.
3. Cross-presentation
- APCs will use the exogenous pathway's endocytosis to redirect antigen to a class I MHC loading and peptide presentation, a process known as cross-presentation.
- Yet, in order for the phenomena of cross-presentation to occur, the internalised antigens must somehow be diverted to a class I loading route from the external system handling class II MHC presentation.
- In the case of dendritic cells, cross-presentation is predominantly seen when it is accomplished by one of the two potential methods.
- According to the first method, cross-presenting cells have unique antigen-processing equipment that permits peptides from external sources to be loaded onto class I MHC molecules.
- According to the second process, cells have specialised endocytosis equipment that sends ingested antigen straight to an organelle, where the peptides are subsequently loaded onto class I MHC molecules.
- The ability of APCs to catch viruses from extracellular settings, process them, and activate cytotoxic T-cell lymphocytes that may target virus-infected cells, which inhibits the propagation of the virus, makes cross-presentation of antigens advantageous.
Antigen-Antibody Complex
- Several antigens are bound to antibodies to create a molecule known as an antigen-antibody complex or immunogenic complex.
- The epitope and paratope components of the antigen and antibody, respectively, govern how well they attach to one another.
- Since antibodies can discriminate between many antigens, they can fight against a variety of diseases.
- The amino acid sequence of the species-specific epitope and paratope determines the extremely particular nature of the interaction between antigens and antibodies.
- An antigen-antibody interaction produces the complex, which is subsequently prone to a variety of reactions such complement deposition, opsonization, and phagocytosis.
- The proportion of antigen to antibody determines the size and form of the immunological complex. The impact of the immunological complex is in turn determined by size.
- Antigen-antibody complexes have developed into a crucial tool for comprehending the interaction between antigens and antibodies and figuring out the mechanisms behind molecular recognition between antibodies and antigens.
- As the attachment of antigen to cell receptors initiates a signalling cascade that activates antibodies, immune complexes also play a part in controlling the generation of antibodies.
- Immune complexes are necessary for a variety of immunological tasks, but their deposition can cause a number of autoimmune disorders, including scleroderma and arthritis.
Antigen Examples
1. Blood group antigens
- Blood group antigens are proteins or sugars that are found on various parts of the membrane of the red blood cell.
- The sugar generated by a variety of processes that catalyse the transfer of sugar units is what makes up the antigens in the ABO blood type.
- The type of enzyme involved, which is in turn defined by the person's DNA, determines the type of sugar in the red blood cell.
- The DNA of the host also determines the proteins that make up the antigens for the Rh blood type. The D antigen, which is present on red blood cells as a large protein, is encoded by the RhD gene.
- Antigen-antibody responses that help differentiate between various blood groups in humans may discriminate between these antigens.
2. Bacterial Capsule
- A polysaccharide layer that is present outside of the cell membrane and causes an immune response in the host is known as a bacterial capsule.
- Being a well-organized coating that is difficult to remove, the capsule is thought to be a potential factor in bacterial pathogenicity.
- Due to the need for a capsule-specific antibody to initiate phagocytosis, the capsule may also play a role in some bacteria's ability to avoid it.
- The polysaccharide component of bacterial capsules is conjugated with protein carriers and utilised as an antigen in vaccinations.
- The exact structure, function, and involvement of capsules in bacteria differ in different bacterial species.
Applications of Antigens
- As antigens are often quite specific, it is possible to distinguish between various bacterial species by looking for specific antigens in distinct species.
- Antibodies may be found in a sample using antigens, which can also be employed as diagnostic tools.
- Antigen-antibody complexes, which are used in forensic applications to identify human blood and other materials, depend on antigens as a key component.
- For the measurement of diverse chemical and biological compounds, they are also utilised in immunoassays.
- Autoimmune illnesses, some of which are fatal, are brought on by autoantigens.
- As a kind of passive immunity, inactivated enzymes are employed in vaccines to treat and prevent many illnesses.