Table of Contents
- Classification
- Habitat
- Morphology
- Cultural Characteristics
- Biochemical Characteristics
- Virulence Factors
- Pathogenesis
- Clinical Manifestation
- Laboratory Diagnosis
- Treatment
- Antibiotic Resistance Profile
- Prevention
Enterococcus faecalis belongs to the Gram-positive, catalase-negative cocci category within the Enterococcus genus. It is non-motile and part of the Enterococcaceae family in the Lactobacillales order under the class Bacilli.
Introduction to Enterococcus faecalis:
- Found as a commensal bacterium in the human gastrointestinal (GI) and vaginal tracts, Enterococcus faecalis is commonly associated with nosocomial infections, including urinary tract infections, wound and soft-tissue infections, bloodstream infections, endocarditis, and meningitis.
- Discovered in 1899 by German microbiologist Fritz Schmalz, Enterococcus faecalis was initially classified as Streptococcus faecalis due to its resemblance to other Streptococcus bacteria. Formerly part of the Group D Streptococci, distinguished by their ability to thrive in bile, it underwent reclassification by the International Council of Microbiologists in 1984. This decision was based on variations in biochemical characteristics, cell wall structure, and genetic data from DNA hybridization studies. The name "Enterococcus" was proposed, derived from the Greek words "enteron" (intestine) and "kokkos" (berry or coccus), leading to the reclassification of the Streptococcus faecalis group as a distinct genus - Enterococcus, with the species S. faecalis reclassified as Enterococcus faecalis.
- Currently part of the 'Enterococcaceae family,' Enterococcus faecalis has emerged as a significant concern in healthcare settings due to its resistance to multiple antibiotics and its capacity to cause various nosocomial infections.
Classification of Enterococcus faecalis
|
Domain |
Bacteria |
|
Phylum |
Firmicutes (Previously Bacillota) |
|
Class |
Bacilli |
|
Order |
Lactobacillales |
|
Family |
Enterococcaceae |
|
Genus |
Enterococcus |
|
Species |
E. faecalis |
Habitat of Enterococcus faecalis
- Enterococcus faecalis demonstrates versatility in adapting and thriving across diverse environments and conditions. Its primary habitat is the intestinal tract of warm-blooded animals, including humans. Additionally, it colonizes the genitourinary tract, particularly the vaginal tract, along with the oral cavity and skin.
- In natural settings, Enterococcus faecalis can be found in soil, water, food, and decomposing vegetation. It is particularly abundant in soil and water contaminated with fecal matter.
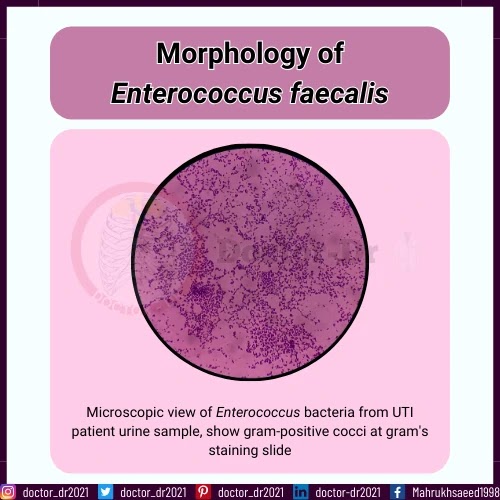
Morphology of Enterococcus faecalis
- Enterococcus faecalis presents as Gram-positive cocci with a slightly oval shape when viewed at higher magnification.
- Typically ranging from 0.5 to 2 μm in diameter, the cells can elongate to 0.6 to 2.5 μm under certain growth conditions, giving them an ovoid appearance.
- Microscopically, these bacteria appear as oval-shaped entities, either as single cells, pairs, or chains.
- They are characterized as non-motile, non-spore-forming, and non-pigment-producing.
- Enterococcus faecalis has the ability to develop pili and form biofilm, enhancing its capacity to colonize and survive in challenging environmental conditions.
Cultural Characteristics of Enterococcus faecalis
- Enterococcus faecalis is a non-fastidious bacterial species, allowing it to thrive on a broad spectrum of general-purpose and selective culture media. As facultative anaerobes, they form visible colonies in temperatures ranging from 10°C to 45°C. These bacteria exhibit resilience to conditions like 6.5% NaCl concentration, bile salts, elevated pH up to 9.5, and even temperatures of 60°C for approximately half an hour. Despite these traits, Enterococcus faecalis is commonly cultivated aerobically at 35 (±2)°C.
- Primary isolation and characterization of Enterococcus faecalis in microbiology labs often employ blood agar medium. Other media such as Nutrient Agar, Bile Esculin Agar, Columbia CNA medium, and MacConkey Agar are also utilized for isolation and identification purposes.
- Selective media specifically designed for the rapid isolation and primary identification of Enterococcus spp., including E. faecalis, include CHROMagarTM Orientation, Brilliance UTI Agar, Enterococcosel agar, and mEnterococcus Agar (Slanetz and Bartley agar).
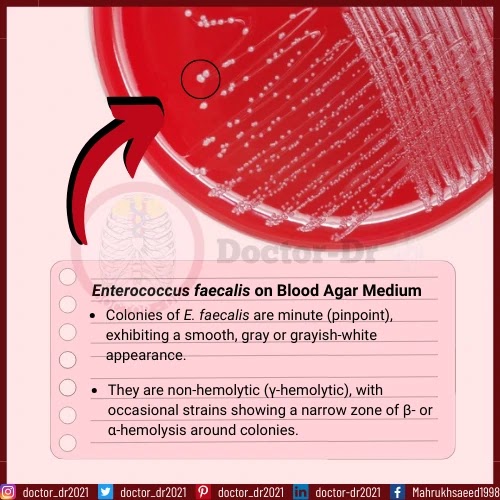
Blood Agar Medium:
- Colonies of E. faecalis are minute (pinpoint), exhibiting a smooth, gray or grayish-white appearance. They are non-hemolytic (γ-hemolytic), with occasional strains showing a narrow zone of β- or α-hemolysis around colonies.
Bile Esculin Agar Medium:
- E. faecalis, being bile salt-tolerant, thrives in 40% bile salt concentration. The colonies are small, convex, transparent, and slightly brownish, often accompanied by a brown-black halo around them. In some cases, blackening of the medium may occur.
Nutrient Medium:
- On nutrient agar, E. faecalis forms small, spherical, smooth, opaque, creamy colonies.
MacConkey Agar Medium:
- On MAC agar without crystal violet, E. faecalis produces small, smooth colonies with pink coloring, indicating its ability to ferment lactose.
Columbia CNA Agar Medium:
- This selective medium for Gram-positive cocci yields small, convex, mostly non-hemolytic, opaque circular colonies with a faint bluish coloration in certain cultures.
Brilliance UTI Agar:
- In Brilliance UTI agar, E. faecalis develops small, circular, smooth colonies with a turquoise blue color.
CHROMagarTM Orientation:
M-Enterococcus Medium (Slanetz and Bartley Agar):
- This selective medium, commonly used for Enterococcus spp. isolation, results in small, circular, smooth, convex colonies with a pink or white color.
Biochemical Characteristics of Enterococcus faecalis
General Biochemical Test Results
|
General Biochemical Characteristics |
Enterococcus faecalis |
|
Arginine dihydrolase Test |
Positive
(+) |
|
40% Bile-salt Tolerance |
Positive
(+) |
|
Bile Solubility Test |
Insoluble |
|
Capsule |
Negative
(-) |
|
Catalase |
Negative
(-) |
|
Citrate (Simmons) |
Negative
(-) |
|
Coagulase |
Negative
(-) |
|
Deoxyribonuclease (DNase) |
Negative
(-) |
|
Esculin Hydrolysis |
Positive
(+) |
|
Gram Staining |
Gram
Positive Cocci |
|
Gas (in MRS broth) |
Negative
(-) |
|
Hemolysis |
γ-
hemolytic (rarely α-and β-) hemolytic |
|
H2S (Hydrogen Sulfide) |
Negative
(-) |
|
LAP (Leucine amino peptidase) Test |
Positive
(+) |
|
Motility |
Non-motile |
|
6.5% NaCl |
Positive
(+) |
|
Nitrate Reduction |
Positive
(+) |
|
Oxidase |
Negative
(-) |
|
OF (Oxidative Fermentation) |
Facultative
Anaerobes |
|
PYR (Pyrrolidonyl Aryl amidase) Test |
Positive
(+) |
|
Pyruvate Broth Test |
Positive
(+) |
|
Spore |
Negative
(-) |
|
Growth at 4°C |
Negative
(-) |
Carbohydrate Fermentation Tests
|
General Biochemical Characteristics |
Enterococcus faecalis |
|
N-Acetylglucosamine |
Positive
(+) |
|
Adonitol |
Negative
(-) |
|
L-Arabinose |
Negative
(-) |
|
D-Arabitol |
Negative
(-) |
|
L-Arabitol |
Negative
(-) |
|
Arbutin |
Negative
(-) |
|
Cellobiose |
Positive
(+) |
|
Dulcitol |
Negative
(-) |
|
D-Fructose |
Positive
(+) |
|
D-
and L-Fucose |
Negative
(-) |
|
Galactose |
Positive
(+) |
|
D-Glucose |
Positive
(+) |
|
Glycerol |
Positive
(+) |
|
Glycogen |
Negative
(-) |
|
Inulin |
Negative
(-) |
|
Lactose |
Positive
(+) |
|
Maltose |
Positive
(+) |
|
Mannitol |
Positive
(+) |
|
D-Mannose |
Positive
(+) |
|
D-Raffinose |
Negative
(-) |
|
Rhamnose |
Variable |
|
Ribose |
Positive
(+) |
|
Sorbitol |
Positive
(+) |
|
Sorbose |
Negative
(-) |
|
Sucrose |
Positive
(+) |
|
D-Tagatose |
Positive
(+) |
|
Trehalose |
Positive
(+) |
|
Tartrate |
Negative
(-) |
|
L-Xylose |
Negative
(-) |
|
D-Xylose |
Variable |
Enzymatic Hydrolysis Tests
|
General
Biochemical Characteristics |
Enterococcus
faecalis |
|
Arginine
Dehydrolase |
Positive
(+) |
|
Caseinase |
Negative
(-) |
|
DNase |
Negative
(-) |
|
Esculin
Hydrolysis |
Positive
(+) |
|
α-Galactosidase |
Negative
(-) |
|
Gelatinase |
Positive
(+) |
|
Lipase |
Positive
(+) |
|
Lysine
Decarboxylase |
Negative
(-) |
|
Leucine
Arylamidase |
Positive
(+) |
|
Ornithine
Decarboxylase |
Negative
(-) |
|
Phenylalanine
Deaminase |
Negative
(-) |
|
Pyrrolidonyl
Aminopeptidase |
Positive
(+) |
|
Tryptophanase |
Positive
(+) |
Virulence Factors of Enterococcus faecalis
Adhesins:
Hemolysin/Cytolysin:
Biofilm Formation:
Gelatinase:
Pathogenesis of Enterococcus faecalis Infections
Adherence and Colonization:
Biofilm Formation:
Release of Toxins and Extracellular Enzymes:
Invasion and Evasion:
Host's Immune Response (Inflammatory Response):
Clinical Manifestation of Enterococcus faecalis
Urinary Tract Infections (UTIs):
Intra-abdominal Infections:
Endocarditis:
Bloodstream Infections:
Surgical Site Infections:
Other Infections:
Laboratory Diagnosis of Enterococcus faecalis:
1. Cultural Characters and Morphological Identification:
2. Biochemical Characterization:
3. Molecular Diagnosis:
Treatment of Enterococcus faecalis Infections
Antibiotic Resistance Profile of Enterococcus faecalis:
- Enterococci exhibit intrinsic and inherited resistance to a broad spectrum of commonly used antimicrobial agents, including aminoglycosides, beta-lactams, and glycopeptides. Reports indicate resistance to widely used therapeutics, including newer options like linezolid, daptomycin, and vancomycin. This extensive antimicrobial-resistant profile poses challenges in treating E. faecalis infections with single antibiotics, necessitating combination therapy and prolonged antibiotic consumption.
- E. faecalis inherently resists several penicillin derivatives. While initially sensitive to ampicillin, the acquisition of beta-lactamase-producing genes and alterations in penicillin-binding proteins (PBPs) have diminished ampicillin's efficacy when used alone or in combination.
- Similarly, E. faecalis has developed resistance against aminoglycosides, macrolides, tetracyclines, and quinolones through the production of aminoglycoside-modifying enzymes, rRNA methylase enzymes, formation of efflux pumps, and alterations in DNA gyrase and topoisomerase-IV, respectively.
Vancomycin-Resistant Enterococci (VRE)/Vancomycin-Resistant E. faecalis (VRE):
- Vancomycin, a reserved antibiotic for E. faecalis treatment, is the drug of choice for beta-lactam-resistant and aminoglycoside-resistant strains. However, global reports indicate emerging resistance to vancomycin by E. faecalis.
- The primary resistance mechanism in E. faecalis involves the acquisition of resistance genes, predominantly vanA or vanB genes. These genes are transferable between various bacterial strains and species, often carried on mobile genetic components like plasmids or transposons.
- The extensive use of vancomycin, particularly in healthcare settings, has exerted selective pressure, leading to the development of Vancomycin-Resistant Enterococci (VRE). Infections caused by VRE strains pose a significant threat, as treatment choices are limited, often requiring combination therapy or newer antibiotics such as linezolid and daptomycin, consequently increasing treatment costs.
Prevention of Enterococcus faecalis Infections:
- Implementation of proper hand hygiene practices.
- Adequate disinfection of equipment.
- Thorough environmental cleaning protocols.
- Isolation of individuals who are either infected or colonized by E. faecalis.





%20-%20Symptoms,%20Treatment,%20and%20Management.webp)

